Nearly half of U.S. adults could now be classified with high blood pressure, under new definitions
By American Heart Association News

ANAHEIM, California -- Nearly half of American adults are at risk for major health problems because of high blood pressure, according to a new scientific guideline that redefines the dangerous condition and provides tactics for doctors to detect, treat and prevent it.
People with readings of 130 as the top number or 80 as the bottom one now are considered to have high blood pressure, according to the guideline released Monday by the American Heart Association. High blood pressure used to be defined as 140/90.
The change means 46 percent of U.S. adults are identified as having high blood pressure, compared with 32 percent under the previous definition. A blood pressure of less than 120/80 still will be considered normal, but levels at or above that, to 129, will be called “elevated.”
The new guideline is designed to help people take steps to control their blood pressure earlier, according to the authors. High blood pressure, also known as hypertension, is a major risk factor for heart disease and stroke – the two leading causes of death in the world.
“Yes, we will label more people hypertensive and give more medication, but we will save lives and money by preventing more strokes, cardiovascular events and kidney failure,” said Kenneth Jamerson, M.D., Ph.D., professor of internal medicine and hypertension specialist at the University of Michigan Health System. He is one of 21 experts on the guideline writing committee. “If you are going to put money into the healthcare system, it’s to everyone’s advantage if we treat and prevent on this side of it, in early treatment.”
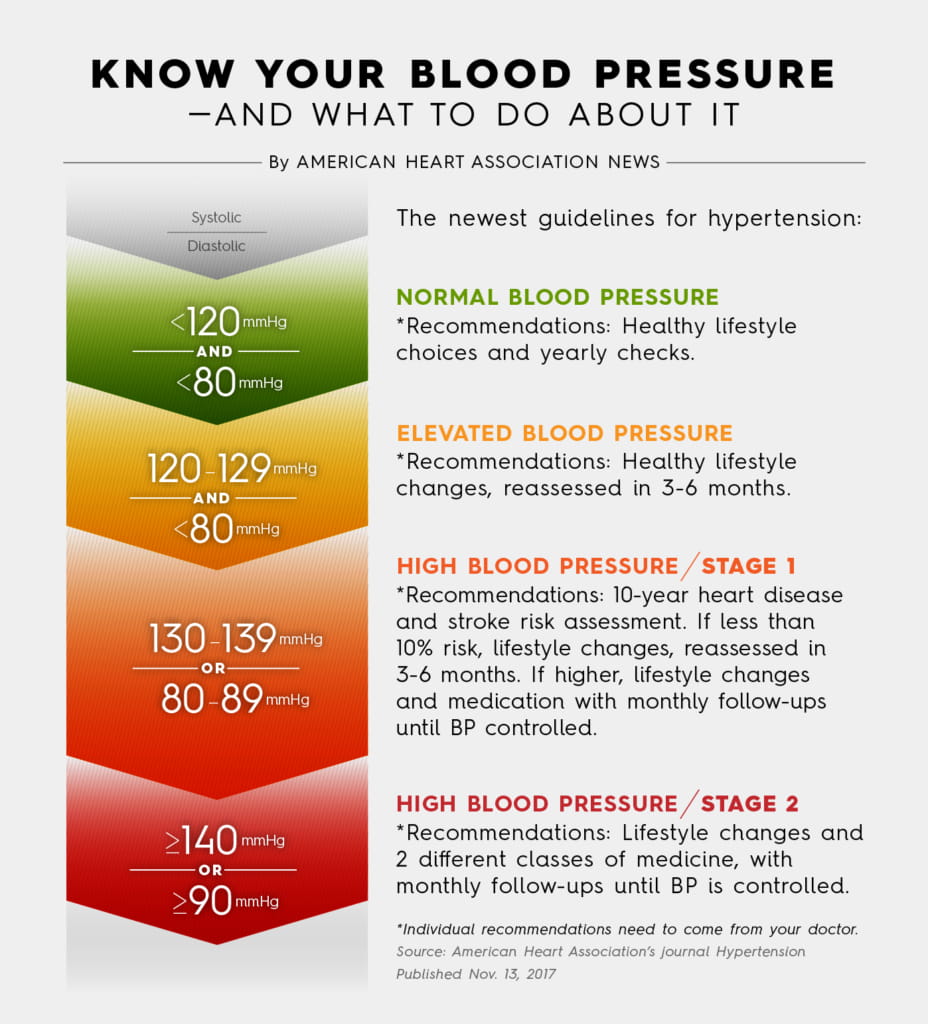
View text version of infographic
Still, the guideline – in the works for about three years and based on hundreds of studies and clinical trials – doesn’t suggest a massive increase in the number of people who will need to take medication to control hypertension.
Of the estimated 14 percent more adults to be classified with high blood pressure, about one in five will need medication, according to Paul Whelton, M.D., who chaired the guideline writing committee. But taking into account the overall population of adults who now will have hypertension, the guide predicts only a small percentage more should be prescribed medicine for it, compared with the previous guideline’s recommendations released in 2003.
Instead, the guideline, published in the AHA's journal Hypertension, emphasizes that doctors need to focus on a whole framework of healthier lifestyle changes for patients.
“We need to send the message that yes, you are at increased risk and these are the things you should be doing,” said Whelton, chair of global public health at Tulane University in New Orleans. “I’m not saying it’s easy to change our lifestyles, but that should be first and foremost.”
The recommendations for a heart-healthy diet include reducing salt and incorporating potassium-rich foods such as bananas, potatoes, avocados and dark leafy vegetables. The guideline also gives specific suggestions for weight loss, quitting cigarettes, cutting back on alcohol and increasing physical activity.
The guideline, the first comprehensive one in 14 years, homes in on making sure doctors’ offices and patients understand how to accurately measure blood pressure and diagnose hypertension in the first place.
Hypertension occurs when the force of blood pushing against vessel walls is too high. This added pressure causes the heart to work too hard and blood vessels to function less effectively. Over time, the stress damages the tissues within arteries, which can further damage the heart and circulatory system.
Often called the “silent killer” because there are often no obvious symptoms, hypertension accounts for more heart disease and stroke deaths than almost all other preventable causes. It’s second only to smoking.
Robert M. Carey, M.D., vice chair of the guideline writing committee, said he expects some controversy over how the report treats older adults. It recommends people 65 and older be treated to the same 130/80 goal as younger patients. A guideline early this year from the American College of Physicians and the American Academy of Family Physicians suggested patients 60 and older be held to a standard below 150/90.
But Carey, professor of medicine and dean emeritus at the University of Virginia School of Medicine, said several intensive studies since 2015 show treating older adults to a lower blood pressure goal is beneficial.
“You have to escalate the treatment slower and monitor any side effects,” he said. “But it’s true there is benefit to treating ambulatory, older subjects.”
The guidelines say it can be lifesaving: “BP lowering therapy is one of the few interventions shown to reduce mortality risk in frail older individuals.” Men and women age 65 to 74 under the new classification will see high blood pressure rates increase by 13 percent and 12 percent, respectively.
Here are how some other groups will be affected by the new measurements:
- High blood pressure rates could nearly triple among men age 20 to 44 – up to 30 percent from 11 percent. Women in that age group will see their rates almost double, to 19 percent from 10 percent.
- Roughly three-quarters of men between 55 and 74 could be diagnosed with high blood pressure.
- Black and Hispanic men will experience a 17 percent increase in rates. Asian men will see a 16 percent increase.
The new classifications and recommendations are specific in how they determine who is at risk and what they should do about it, Jamerson said.
Doctors should use a “risk calculator” to determine a patient’s risk of heart disease or stroke over the next 10 years. That assessment, combined with the other recommendations, can prompt more thorough doctor-patient conversations to determine whether lifestyle changes alone can help, or if medicine is needed as well.
“These new guidelines give patients a voice because it gives them an opportunity to ask healthcare providers, ‘What’s my risk?’” Jamerson said. “Consumers should be getting an explanation. Physicians ought to be calculating risk as they think about how to treat."
If you have questions or comments about this story, please email [email protected].





