Dr. Helen Taussig's work saved 'blue babies' and made her the mother of pediatric cardiology
By Laura Williamson, American Heart Association News

Before Dr. Helen Taussig came along, pediatric cardiology didn't exist.
Babies born with heart defects often turned blue and died. She helped them to live.
Before Taussig spoke up, a morning sickness drug, which caused birth defects in thousands of babies in Europe, was being considered for mass distribution in the U.S. She helped keep it out.
Before Taussig, every president of the American Heart Association was a man.
She opened the door to women.
And then Taussig leveraged her position to bring greater attention to pediatric cardiology worldwide.
"She had a reputation as a lifelong advocate for pediatric health," said Dr. Laura Olivieri, director of noninvasive cardiac imaging and an associate professor of pediatrics at the University of Pittsburgh Medical Center in Pennsylvania. "But she was somewhat controversial at the time."
By all accounts, she also was fiercely determined.
Overcoming early obstacles
Born in 1898, Taussig's early years were littered with obstacles. Her mother died from tuberculosis when Taussig was just 11 years old, and her own milder case left her frail. She struggled with dyslexia, which made it difficult for her to read. A bout with whooping cough damaged her hearing, a problem that would grow progressively worse as she got older.
But Taussig, the youngest of four children, was encouraged by her father, a world-renowned Harvard economist, to persevere. She did, finding shortcuts, triple-checking her work and ultimately excelling at school. She spent two years at her mother's alma mater, Radcliffe College in Cambridge, Massachusetts, before transferring to and graduating in 1921 from the University of California, Berkeley.
After college, Taussig was determined to become a doctor, despite the fact that women were largely excluded from the field. Harvard offered to let her take classes but wouldn't confer a medical degree to a woman. So, she went to Johns Hopkins University in Baltimore, which admitted women from day one.
Taussig ran into another wall at graduation, however, when she narrowly missed earning a coveted residency in internal medicine at Johns Hopkins Hospital. After working for a year in an adult heart clinic, she took a residency in pediatrics instead and began volunteering at a children's heart clinic run by Dr. Edwards Park, at the Harriet Lane Home for Invalid Children.
That twist of fate changed everything.
Blue babies
Taussig ultimately took over running the clinic, where she stayed until her retirement in 1963. There, she treated children whose hearts were weakened by rheumatic fever as well as those with a wide range of heart defects.
Because of her hearing loss, Taussig had difficulty using a stethoscope. Instead, she felt the vibrations of their heartbeats using her hands, learning to diagnose their conditions based on what she felt. As new technology became available, in particular a portable type of X-ray known as a fluoroscope, she added these to her arsenal of diagnostic tools.

She also learned a great deal about how baby's hearts worked – or failed – by performing autopsies on them.
In the 1940s, most children born with heart defects were thought untreatable and sent home to die. But Taussig figured out that the problem with "blue babies," a condition known as cyanosis, was that they weren't getting enough oxygen because there wasn't enough blood going to their lungs. She thought it might be possible to fix that by connecting an artery leading to the heart to one leading to the lungs.
She persuaded Hopkins' chief surgeon, Dr. Alfred Blalock, that it could be done. Blalock's surgical assistant, Vivien Thomas, helped figure out how. The first successful Blalock-Taussig-Thomas shunt operation was performed on a 2-year-old girl in November 1944.
That groundbreaking procedure not only saved children's lives, it also paved the way for the development of adult open-heart surgery, said Dr. Thomas Traill, director of the E. Cowles Andrus Cardiac Clinic and a professor of medicine in the cardiology division at Johns Hopkins University.
"Until she came up with the notion that we could improve blood flow to the lungs by creating a shunt and Blalock and Thomas figured out how to do it, there was no such thing as pediatric cardiac surgery or pediatric cardiology," he said. "She introduced the idea that you could make a change in circulatory physiology."
The Blalock-Taussig-Thomas shunt procedure was performed on nearly 900 children by the end of the 1940s alone, and it has since saved thousands of lives. Though it has evolved over the years, the procedure is still used today.
Traill, who took over at the adolescent clinic with patients who had once been cared for by Taussig, was a cardiology student in London when he learned about her work at Johns Hopkins.
"I recognized that this would be an interesting place to see young patients with this condition, because this was where it all began" he said. Taussig took her work with children with heart disease at the clinic, "and turned it into a place where children came from all over the world and got better."
Fighting thalidomide
Taussig was equally persuasive about the need to ban thalidomide, a drug used to relieve pregnancy-related morning sickness in the 1950s and '60s that many believed was harmless. In the early 1960s, she went to Europe to speak personally to women whose babies developed debilitating birth defects after they took the drug and returned to share their stories with the Food and Drug Administration.
Along with FDA reviewer Dr. Frances Oldham Kelsey, Taussig's diligence prevented the drug from being distributed in the U.S. (Thalidomide was later approved by the FDA to treat leprosy and multiple myeloma, with a warning label that the drug can cause severe birth defects.)
Her work earned her the presidential Medal of Freedom in 1964. The following year, Taussig was asked to become the first woman president of the AHA.
Under her leadership, she broadened the AHA's focus on prevention to include children, advocating for healthier childhood diets to prevent arteries from hardening during adulthood.
Olivieri never met Taussig, who died in a car crash in 1986, just days before her 88th birthday. But Taussig's pioneering work in pediatric cardiology was so legendary, it has resonated with Olivieri since she first learned about Taussig in medical school.
"As I understand it, she was a big personality among other big personalities at the time," said Olivieri, who serves on the AHA's Young Hearts Congenital Heart Defects Committee. "Most of us in the field are in awe of her. I love thinking about what she had to do to get people on board with her vision. She really moved the needle both for children with congenital heart disease and for women in academic medicine."

Devoted to trainees and children
Taussig was also known for developing a pediatric cardiology training program and her devotion to the doctors she mentored.
Traill met several of them, though Taussig had retired by the time he got to Johns Hopkins. "They really worshipped her," he said.
The feeling was apparently mutual.
"Her devotion to her trainees was quite remarkable," said Dr. Anne Murphy, a retired pediatric cardiologist who worked alongside one of Taussig's mentees, Dr. Catherine Neill, at Johns Hopkins. Murphy recalls Neill speaking highly of her mentor and was present a few times when Taussig returned to attend meetings. Everybody gravitated to her, she said, even though Taussig's hearing loss made conversations challenging.
"There isn't a pediatric heart surgeon today who doesn't appreciate the work she did," Murphy said.
Traill himself has an affection for Taussig, keeping some of her old patient files, along with her meticulous notes, in a corner of his office. "She wrote beautiful, accurate, detailed notes," he said. They often included personal advice to parents, in one case encouraging them to "have another child."
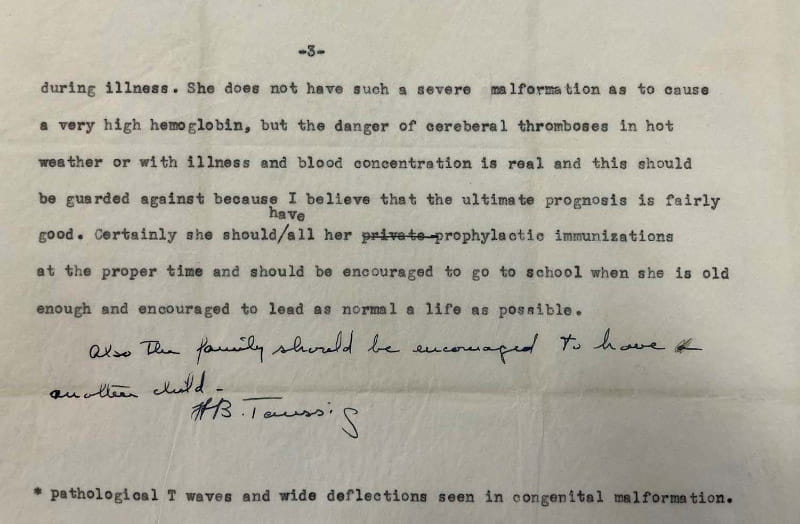
"I will go to my grave wondering if she meant that the child she was treating would not survive so they should have another one, or that they shouldn't worry about having another child because the condition doesn't run in families," he said.
Artists and photographers who tried to capture Taussig for posterity invariably missed the mark, he said. In one widely used photo, Taussig is holding an infant in her arms, smiling warmly at the babe while listening to its heart with a stethoscope. Not only is the stethoscope out of place, since the instrument held little use for her, the feeling the image evokes is off base, Traill said.
"She was not the cozy, cuddly woman depicted holding a child in her lap," said Traill, who met Taussig at Johns Hopkins events. "Of course she did that, held the babies, but in practice she was reserved, very pragmatic. She was not the snuggly bunny that is so easy to portray with pediatricians."
"It's a little saccharine," he said. "She was not a saccharine person."

But that doesn't mean she wasn't devoted to her patients, he said.
"Her patients recognized her complete devotion to them. They were a little bit in awe, but mostly in love," he said. "Despite a certain natural reserve, she allowed people to understand how much she was involved and cared about them."
In contrast, in a portrait painted by Jamie Wyeth, the son of renowned American artist Andrew Wyeth, she appears overly stern. The portrait, commissioned by cardiologists trained by Taussig, was so dark, it was met with gasps when it was unveiled. It was later given to Taussig, who stuck it in an attic where it sat under wraps for decades.
Her great-nephew, George Henderson, remembers his father being at a loss regarding what to do with the portrait when they cleaned out her home after her death. But the painting, which the family ultimately returned to Johns Hopkins, was a far cry from the woman Henderson remembered from his childhood and young adult years.
"It was a striking portrait, and she was a striking woman," he said. "But it was unlike anything I ever visually experienced of her."
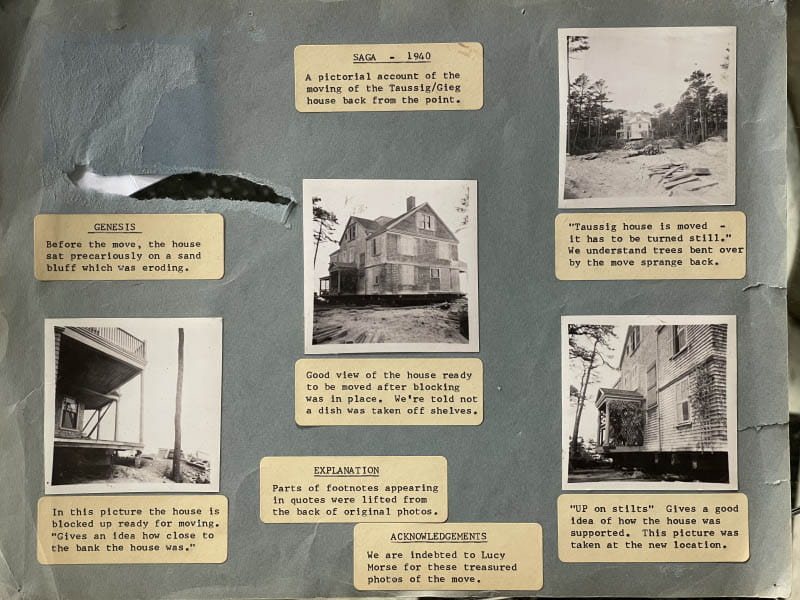
Henderson remembers his great-aunt as a somewhat distant but professional woman who graciously welcomed family to her summer home on Cape Cod in Massachusetts, where the family vacationed for generations. He grew up swimming in the lagoon off her beach in Cotuit. Aunt Helen, who was in the habit of waking up early, started each day with a swim in the cold Cape waters – in the buff. By the time everyone else woke up, she was in the kitchen making coffee. She ended her day by sleeping outdoors on the porch.
That was one habit Taussig never changed, Henderson said. Even after moving to Pennsylvania in her 80s, she moved her bed onto her porch and had it screened in so she could sleep there. She had to climb through a window to get to it.
Henderson said he was unaware of his great-aunt's legacy as a child and is still learning things about her from her biographers. "By the time I was in college, I knew she was renowned," he said. "But it wasn't terribly meaningful to me then." It is now.
Taussig's legacy is every medical student's dream, said Olivieri, who pointed out that congenital heart defects affect 1 in 100 babies and "about 25% of them will need some intervention before age 1 to extend their life."
"That's a lot of babies," she said. "And there were no treatments, nothing that medicine could offer them before Taussig's time. She gravitated toward this population of children and babies who had no options, and she gave them an option that was totally lifesaving. How can you do any better work than that?"





