The chaotic beginnings of the tool that made heart surgery possible
By Michael Merschel, American Heart Association News

Over the past century, heart operations that once were unthinkable have become commonplace. Thousands of times a day, surgeons graft arteries, fix structural defects or transplant entire hearts.
Procedures like these are possible because medical teams can stop a patient's heart, pump their blood with a machine during surgery, and restart the repaired heart afterward.
The development of that process, commonly called heart-lung bypass, is a triumph of science and engineering that involved taking risks in ways that would be unthinkable today. Desperate surgeons took those risks because the stakes were enormous: People, often children born with heart defects, were dying. Surgeons knew they could save lives, if only they could access the heart's interior.
The creation of heart-lung bypass was clearly "one of the major milestones of modern medicine," said Dr. James K. Kirklin, the former director of cardiothoracic surgery at the University of Alabama at Birmingham, who now leads a company spun off from the school. He co-wrote a 2022 article in the Journal of the American College of Cardiology on how heart-lung bypass was developed.
The effort involved "tremendous collaboration" among researchers, he said. They were driven to work together by "about as pure a motivation as you could possibly have" – the hope of giving children facing certain death the prospect of a full lifespan. "I mean, who would not want to collaborate on this kind of project?"
The beginnings
The full history of heart-lung bypass dates back to at least the late 1800s, when German scientists learned how to infuse blood with oxygen by passing it through a membrane. The modern story might begin with Dr. John H. Gibbon Jr. As a research assistant at Massachusetts General Hospital in 1931, he was assigned to watch over a woman dying of a blood clot in her lungs, known as a pulmonary embolism. She succumbed during an emergency attempt at surgery.
Gibbon later told of how "during the 17 hours by the patient's side, the thought constantly recurred that the patient's hazardous condition could be improved if some of the blue blood in the patient's distended veins could be continuously withdrawn into an apparatus where the blood could pick up oxygen and discharge carbon dioxide, and then pump this blood back into the patient's arteries."
Colleagues thought it was a bad idea. "The general impression was that it would in all probability be a monstrous waste of the time and energy of a bright young investigator to embark on such an almost impossible task," said his wife, Mary "Maly" Hopkinson Gibbon, as quoted by the Science History Institute of Philadelphia. She became an important collaborator.
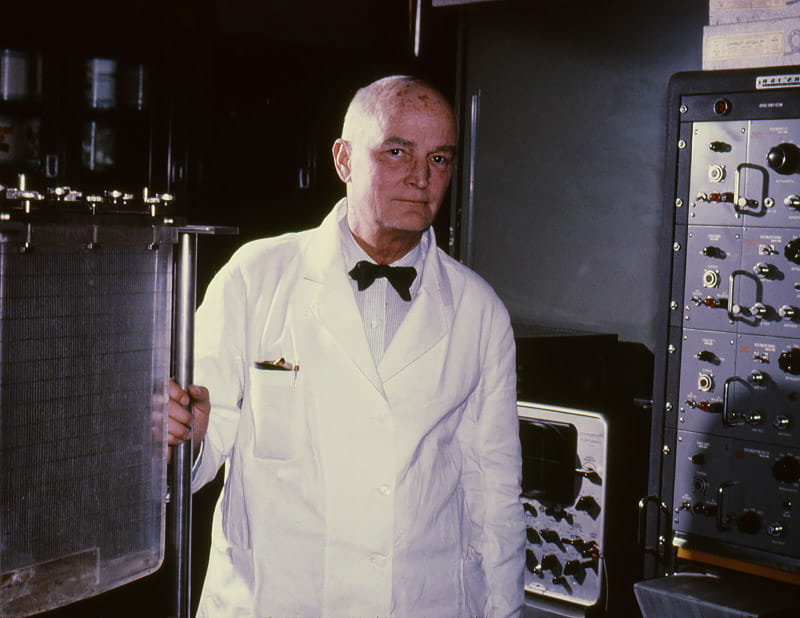
After serving in World War II, Gibbon ended up as a social acquaintance of Thomas J. Watson, who provided engineering help from IBM, where he was chairman of the board. The heart-lung device that resulted drew comparisons to a punch-card machine.
The war had helped teach surgeons that, contrary to conventional wisdom of the day, it was possible to repair a heart. "Basically, the philosophy before World War II is you couldn't work on the heart without grave risks to the patient," said Dr. Paul A. Iaizzo, a professor of surgery at the University of Minnesota in Minneapolis, where he leads the Visible Heart Laboratories.
The war was also where Dr. Wilfred G. Bigelow of Canada, who had been treating soldiers for frostbite, became interested in the effects of hypothermia, which can slow the body's metabolic rate and decrease its need for oxygen. Before heart-lung machines were available, some early heart operations were made possible just by cooling patients, which gave surgeons a brief window to operate.
All the pieces of the puzzle started to come together in Minnesota in the early 1950s. To grasp how groundbreaking the pieces were, it helps to understand the relatively primitive conditions surgeons then worked under.
"There's no computers or digital equipment," Iaizzo said, and no electronic sensors. Body temperatures were recorded with glass thermometers. Pulses were checked by hand as someone watched a clock on the wall. To induce hypothermia, patients were packed in ice and set inside the type of metal trough used to provide water to horses. Anesthesia was regulated by hand-pumping a bag and was sometimes explosive.
There were no effective defibrillators, which made the cooling process dangerous. And hearts could start beating erratically as they were warmed up.
Doctors worked blind, save for a static chest X-ray that would have been taken outside the operating room; there were no portable X-ray machines or other imaging devices.
"They're making this up as they went," Iaizzo said, adding that doctors had valid reasons for being "mavericks" given how deadly the situations could be.
As bypass techniques were tried on desperately ill patients, the early fatality rates were correspondingly high. "The initial numbers were just disastrous," Kirklin said.
But doctors kept trying.
Failing and trying again
In 1952, Gibbon, then at Thomas Jefferson Medical College in Philadelphia, used a heart-lung machine to operate on a 15-month-old who was thought to have an atrial septal defect, where a baby is born with a hole inside the heart. The diagnosis was wrong, and the child died.
On May 6, 1953, Gibbon tried again, this time to repair an atrial septal defect in 18-year-old Cecelia Bavolek. She was placed on a heart-lung machine for 45 minutes. The procedure worked, and Gibbon is credited with performing the first successful cardiac operation using a mechanical heart-lung machine.
"The machine is not a cure-all for all heart conditions," he told Time magazine in the days after the procedure. But for the first time, "it is possible to look into the heart. It's sort of like drying out a well to do some work at the bottom of it."
Unfortunately, Bavolek was the lone survivor out of four to six attempts. At that point, doctors were pessimistic that open-heart surgery could ever work. Gibbon stopped doing heart surgeries and turned plans for his machine over to a group at the Mayo Clinic in Rochester, Minnesota.
"He was a wonderful gentleman, a superb thoracic surgeon and obviously an innovator, but he was not interested primarily in heart surgery," Kirklin said.

Meanwhile, in the very building where Iaizzo works now, Dr. Owen Wangensteen ran a surgical department where he required his doctors to earn Ph.D.'s, Iaizzo said. It created a culture where innovation was prized, and in an era with no federal oversight of medical devices, it was possible for doctors to come up with an idea, do "three or four experiments in the lab, and go upstairs and try it on a human," he said.
Regulations today provide important safety measures, Iaizzo said. But that era prioritized speed.
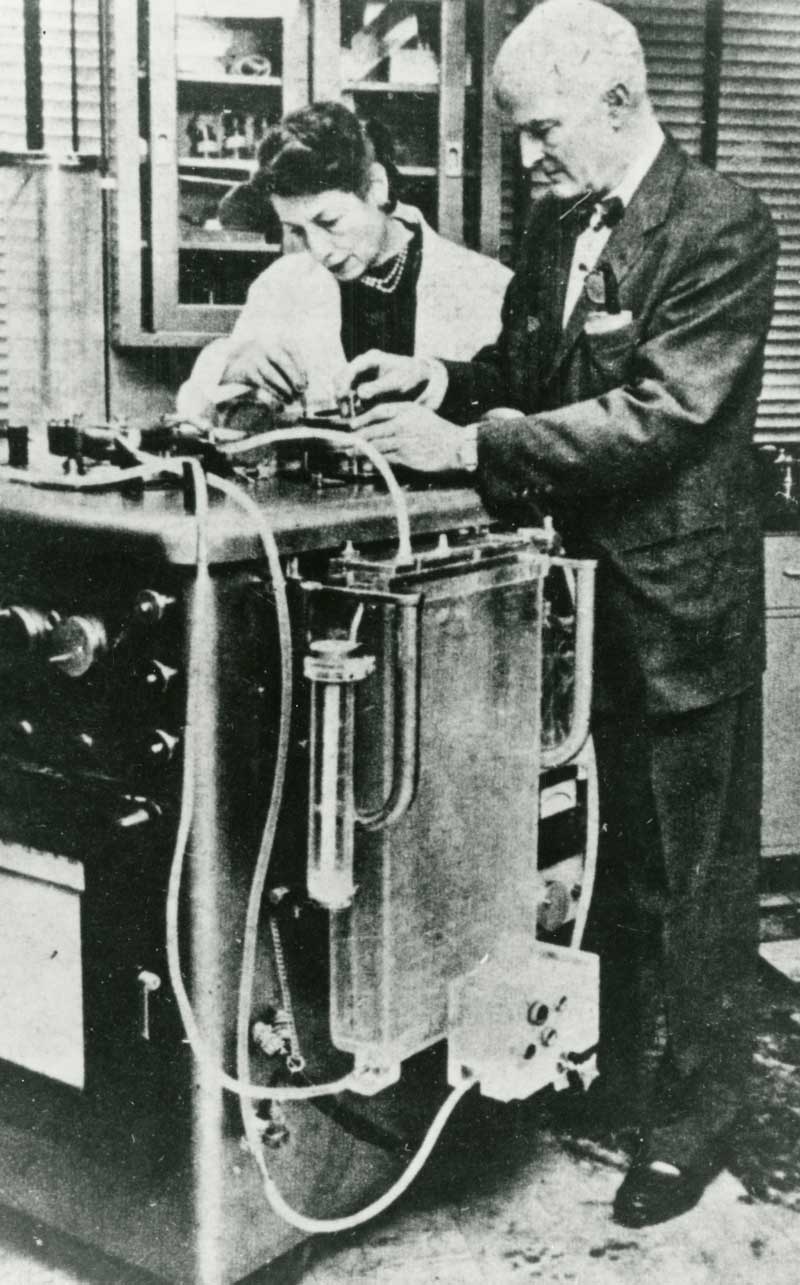
One of the Minnesota physicians, Dr. C. Walton Lillehei, and colleagues worked out a technique called cross-circulation. Blood would be pumped between a young patient and an adult, usually a parent, while surgeons attempted to repair the child's heart. The parent, in effect, served as the heart-lung machine for their child.
The first successful operation using this technique was March 26, 1954. The child, a 13-month-old with a defective ventricle (one of the heart's lower chambers), died 11 days later from pneumonia. But a second child, a 3-year-old with a similar defect, lived for 64 years.
Lillehei would use cross-circulation 45 times; 28 of the patients survived. "A couple of those patients are still alive today," Iaizzo said.

But cross-circulation had limits, Kirklin said. Significantly, it came with the possibility of a 200% mortality rate – the deaths of both child and parent.
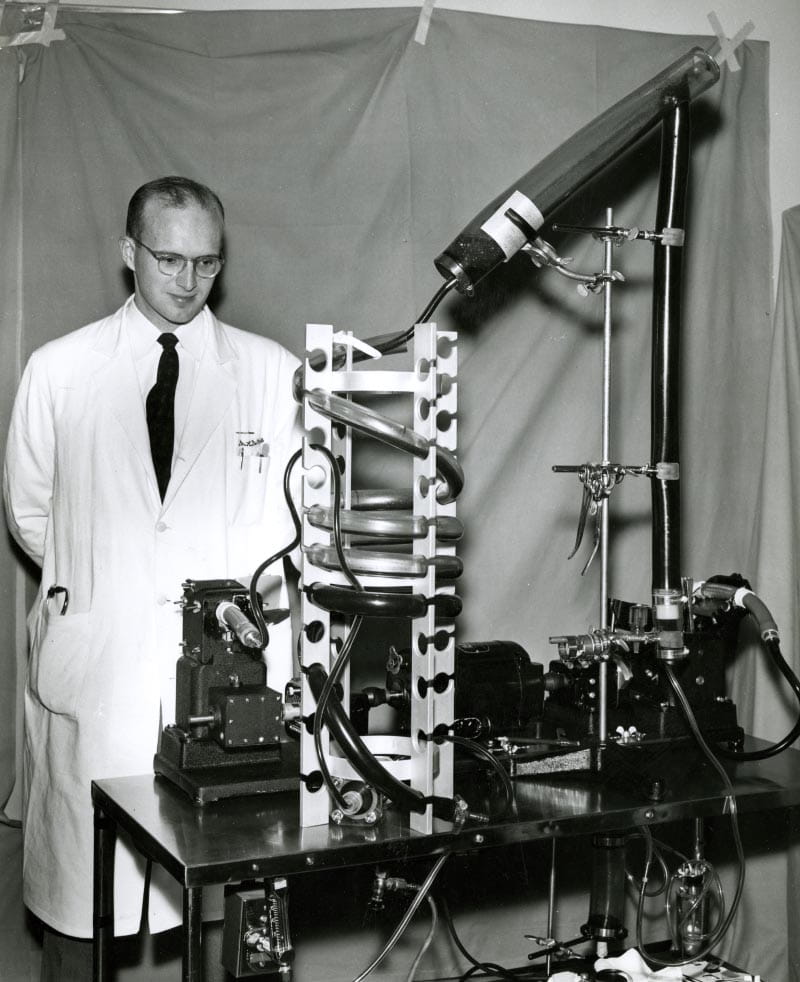
So down the road in Rochester, a team was taking Gibbon's model and refining it. Among the leaders of the effort was Kirklin's father, Dr. John W. Kirklin.
After successful experiments, the Mayo team received permission from their board of governors to attempt to use the machine in eight surgeries, even if the first seven died. The surgeries began in March 1955.
The first patient, a 5-year-old girl with a ventricle defect, survived. "Overall, half of those cases survived, which was quite amazing," Kirklin said. It was the world's first series of successful open-heart operations using cardiopulmonary bypass. "And then things exploded."
Part of the success of heart-lung bypass at this point came from the fact that the surgeons involved were not generalists, Kirklin said. "Walt Lillehei and my father really were the first two cardiac surgeons whose primary focus during this pioneering period was on the heart itself." So when surgeons began those initial eight cases, "they knew exactly what they were planning to do."
Once successful operations had been demonstrated, "there was no turning back," Kirklin said. The Mayo-Gibbon device was the most widely used heart-lung machine of the 1950s and early 1960s.
Back in Minneapolis, cross-circulation was abandoned. University of Minnesota surgery instructor Dr. Richard DeWall had been working on a heart-lung machine that used polyvinyl tubing that kept bubbles from forming in the blood. Lillehei had learned about the tubing from a friend in the food business, where it had been used to make mayonnaise.
The first operation using this machine was performed in May 1955. It cost less than $1,000 to assemble, and its design was used through the 1970s.
"It really transformed cardiac surgery around the world," Iaizzo said.
Although many others contributed to the development of bypass technology, there's no question that the developments made Minnesota the epicenter of open-heart surgery. In 1955 and 1956, the only places offering such surgeries were about 90 miles apart, in Minneapolis and Rochester.
Writing in 2011 in the Journal of Thoracic and Cardiovascular Surgery, DeWall said that happened in part because of collaboration among researchers. "A free exchange developed between the teams of Dr. (John) Kirklin and Dr. Lillehei about their increasing experience in open heart surgery. Members from the Minneapolis team visited the Mayo Clinic, as did Mayo Clinic personnel visit the University of Minnesota's open heart surgery program."

Bypass today
When it comes to heart surgery, things can never be "routine," said Dr. Leora Balsam, a professor at UMass Chan Medical School in Worcester. Patients, she said, "are counting on you to make sure that they come out of this better than they started. That heart has to start up again afterwards."
But heart-lung bypass is so common now that Balsam, who's also surgical director of the ventricular assist device program at UMass Memorial Medical Center, has performed procedures using it more times than she can count. "Maybe a few thousand," she estimated.
For each procedure, Balsam connects a large tube, usually to the upper right chamber of the patient's heart, to pump out blood. The bypass equipment then filters out carbon dioxide and adds oxygen. Blood goes back through another tube that she's connected, usually to the patient's ascending aorta, the large vessel that carries blood from the heart to the rest of the body.
The machine has a heat exchanger that allows her to regulate blood temperature. So before a heart is stopped, she can cool a patient to limit their heart's metabolic needs.
To stop the heart, she clamps off the arteries that provide the heart muscle itself with blood, then injects a potassium solution that stops the heart's electrical activity. "The heart then becomes motionless and electrically quiet. Inactive. Flatlined," she said.
Repairing the heart can take less than an hour, or it might take several. Time matters. Components of the blood can become diluted or stick to the tubing as it circulates. The less time the heart is stopped, the better. "If the heart starts off strong, it can put up with more time. If the heart is weak, it can't handle as much," Balsam said.
When the repairs are done, she restores normal blood flow to the heart's arteries, which washes out the potassium solution and reawakens the electrical beat.
The process has become safer over time, Balsam said. Formulations of the heart-stopping fluid have been improved, and future progress, she said, might lie in making equipment that causes less damage to the blood as it's pumped.
A simplified type of heart-lung bypass called ECMO, which stands for extracorporeal membrane oxygenation, was developed in the 1970s. It has been used to support patients with severe heart and lung complications.
Kirklin said that, as with other complex medical breakthroughs, heart-lung bypass exists because of a combination of "opportunities, serendipity, skill and preparation that led to success."
But he echoed Balsam in saying that even as the machines turned what was once impossible into an everyday occurrence, cardiac surgery is hardly routine. "It needs to be routine from the patient's point of view and from the public point of view," he said, "but not from those who are responsible for the outcome."
Kirklin likened it to flying jets or sending astronauts into space. "Just because they do it safely does not mean it's easy."





