Ablation for Arrhythmias
Catheter ablation is a procedure that uses radiofrequency energy (similar to microwave heat) to destroy a small area of heart tissue that is causing rapid and irregular heartbeats. Destroying this tissue helps restore your heart’s regular rhythm. Catheter ablation destroys the abnormal tissue without damaging the rest of the heart. The procedure is also called radiofrequency ablation.
Why do people have catheter ablation?
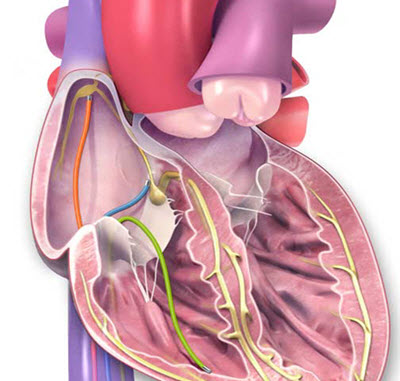
Special cells in your heart create electrical signals that travel along pathways to the chambers of your heart. These signals make the heart’s upper and lower chambers beat in the proper sequence. Abnormal cells may create disorganized electrical signals that cause irregular or rapid heartbeats called arrhythmias. When this happens, your heart may not pump blood effectively and you may feel faint, short of breath and weak. You may also feel your heart pounding.
Medications are used to treat rapid and irregular heartbeats in many people. But they don’t work for everyone, and they may cause side effects in some people. In these cases, catheter ablation may be suggested. The procedure is used most often to treat a condition called supraventricular tachycardia, or SVT, which occurs because of abnormal conduction fibers in the heart. Catheter ablation is also used to help control other heart rhythm problems, such as atrial flutter and atrial fibrillation.
What are the risks?
This procedure is generally safe. Complications are rare but may include:
- Arrhythmias
- Bleeding where the catheter is inserted
- Infection
- Blood clots
- Heart or blood vessel damage
- Damage to the artery where the catheter was inserted
How should I prepare for the procedure?
- Your health care professional will tell you what to eat and drink during the 24 hours before the test.
- You’ll be asked not to eat or drink anything after midnight the night before the procedure.
- Tell your health care professional about any medications you take. They may ask you not to take them before your test. Don’t stop taking your medications until you are asked to.
- Leave all your jewelry at home.
- Arrange for someone to drive you home after your procedure.
What happens during catheter ablation?
A doctor with special training performs the procedure along with a team of nurses and technicians. The procedure is done in a hospital electrophysiology (EP) or cath lab.
- A nurse will put an IV into a vein in your arm so you can get medication (anesthesia) to prevent pain. You may also get a medication (sedative) to help you relax, but you will be awake during the procedure.
- The nurse will clean and shave the area where the doctor will be working. This is usually in your groin.
- The nurse will give you a shot (a local anesthetic) to numb the needle puncture site.
- The doctor will make a needle puncture through your skin and into the blood vessel (typically a vein, but sometimes an artery) in your groin, arm, neck or upper thigh. A small straw-sized tube (called a sheath) will be inserted into the blood vessel. The doctor will gently guide a catheter (a long, thin tube) into your vessel through the sheath. A video screen will show the position of the catheter. You may feel some pressure in your groin, but you shouldn’t feel any pain.
- The doctor will insert several long, thin tubes with wires, called electrode catheters, through the sheath and feed these tubes into your heart.
- To locate the abnormal tissue causing arrhythmia, the doctor will send a small electrical impulse through the electrode catheter. This activates the abnormal tissue that is causing your arrhythmia. Other catheters record the heart’s electrical signals to locate the abnormal sites.
- The doctor will place the catheter at the exact site inside your heart where the abnormal cells are. Then, a mild, painless radiofrequency energy (similar to microwave heat) is sent to the tissue. This destroys heart muscle cells in a very small area that are responsible for the extra impulses that cause your rapid heartbeats.
- Catheter ablation can take four hours or longer. Your doctor will determine if you may go home the same day or if you have to stay overnight.
What happens after catheter ablation?
You’ll be moved to a recovery room and monitored. The sheath usually stays in your leg for several hours after catheter ablation. During this time, you have to lie flat.
After the doctor or nurse removes the sheath:
- A nurse will put pressure on the puncture site to stop the bleeding.
- You should keep your leg straight for several hours after the doctor or nurse removes the sheath. You will be told when you can get out of bed.
- Your heartbeat and vital signs (pulse and blood pressure) will be monitored.
- Tell your doctor or nurse right away if you notice any swelling, pain or bleeding at the puncture site or if you have chest pain.
- Before you leave the hospital, you’ll be given written instructions about what to do at home.
- Along with your regular medications, you may be prescribed others to assist in your recovery after the procedure.
What happens after I get home?
Follow the instructions you were provided before leaving the hospital. Most people can return to their normal activities the day after they leave the hospital, with a few exceptions. For the first week after the procedure:
- Don’t drive until your health care professional says you can.
- Avoid heavy physical activity until your health care professional says it’s safe.
- Don’t lift anything weighing more than 10 pounds.
- Don’t take a bath, swim or otherwise submerge the incision site in water.
- Keep the incision site clean and dry. Call your health care professional if you notice any signs of infection.
- If the site starts to bleed, lie flat and press firmly on top of it. Have someone call your health care professional or hospital.
Call 911 if:
- A lump develops by puncture site, indicating a hematoma
- Bleeding from the puncture site does not slow down when you press on it firmly
- You feel pain or discomfort in your chest that moves into your neck, jaw or arm
- Face drooping, arm weakness, speech difficulties
Call your health care professional if:
- Your leg with the puncture becomes numb or tingles, or your foot feels cold or turns blue.
- The area around the puncture site looks more bruised.
- The puncture spot begins to swell, or fluids drain from it.
- You feel sick to your stomach or sweat a lot.
- You have a fast or irregular heartbeat.
- You feel short of breath.
- You feel dizzy or lightheaded enough to have to lie down.
View an Answers by Heart sheet: What Are Electrophysiology Studies? (PDF)





